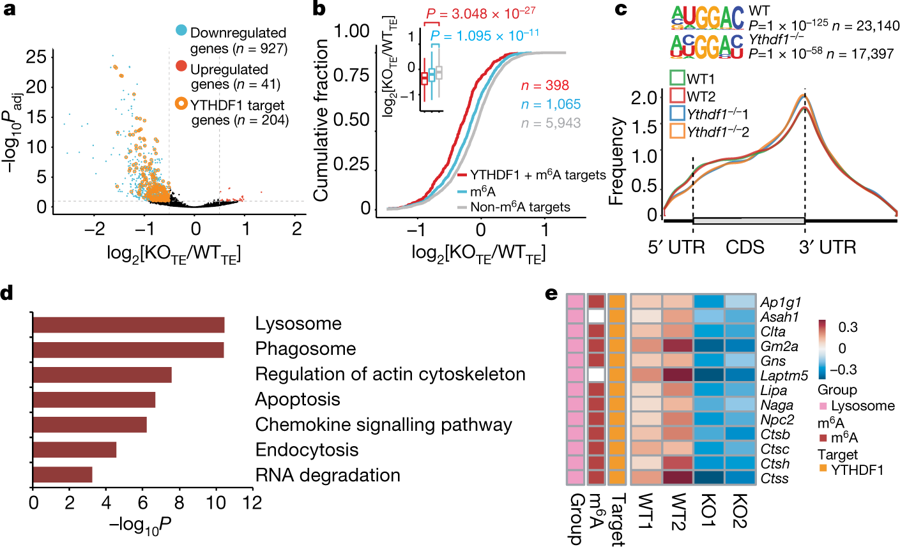
Spontaneous T cell priming against tumor neoantigens is critical for the clinical efficacy of immunotherapies. However, in many patients, neoantigen recognition is insufficient to induce the lasting T cell response required for complete tumor rejection. Identifying molecular pathways that influence the immunoreactivity to tumor neoantigen could provide new targets for improving the response to immunotherapy. HAN Dali’s group in Beijing Institute of Genomics, Chinese Academy of Sciences, cooperating with Meng Michelle XU’s group in Tsinghua University and HE Chuan’s group in University of Chicago, has revealed how the messenger RNA (mRNA) N6-methyadenosine (m6A) methylation affect antigen-specific CD8+ T cell antitumor response by regulating translation of lysosomal cathepsins in dendritic cells. This work has been published in Nature on Feb 6. m6A is the most abundant internal mRNA modification and responsible for posttranscriptional regulation of mRNA in diverse cell types. m6A can affect mRNA translation efficiency via the m6A-binding protein YTHDF1. Dysregulation of m6A pathway components could affect oncogene expression, revealing a link between m6A and tumorigenesis. As most studies focus on tumor intrinsic oncogenic pathways, potential roles of the mRNA m6A modification in host antitumor immune response are unknown. In this work, HAN Dali and his colleagues show that durable neoantigen-specific immunity is regulated by RNA m6A methylation through the m6A-binding protein YTHDF1. In contrast to wild-type mice, Ythdf1-deficient mice exhibit an elevated antigen-specific CD8+ T cell antitumor response. Loss of YTHDF1 in classical dendritic cells enhanced the cross-presentation of tumor antigen and the cross-priming of CD8+ T cells in vivo. Mechanistically, transcripts encoding lysosomal proteases are marked by m6A and recognized by YTHDF1. Binding of YTHDF1 to these transcripts elevates translation of lysosomal cathepsins in DCs, with the inhibition of cathepsins ma. Furthermore, the researcher revealed that the PD-L1 expression was increased in tumour cells from Ythdf1-/- tumour-bearing mice compared with wild-type mice. The therapeutic efficacy of PD-L1 checkpoint blockade is enhanced in Ythdf1-/- mice. In line with the observations in mouse models, the researchers also found that patients with colon cancer who had low expression of YTHDF1 in the tumour stroma tended to have a higher number of CD8+ cells in tumour biopsies, further supporting the notion that the reduced YTHDF1 expression may correlate with the T cell inflamed tumour microenvironment. These data suggest that combining a checkpoint blockade with YTHDF1 depletion could be a potential new therapeutic strategy to improve outcomes in patients with low response to checkpoint blockade. Transcriptome-wide identification and analysis of YTHDF1-binding sites (Image by HAN Dali's group) Contact: Dr. HAN Dali Email: handl@big.ac.cn CAS Key Laboratory of Genomic and Precision Medicine